Parkinson’s and diabetes

Diabetes is a chronic condition affecting 4.5 million people in the UK. Research indicates there is a relationship between Parkinson’s and diabetes, with some recent data suggesting treatment or prevention of diabetes may also reduce the risk of Parkinson’s or affect the progression of the condition.
What is diabetes?
Diabetes is a medical condition where blood sugar levels (or glucose) in the body are too high. We all need glucose – it is a source of energy for our bodies to function properly. Our bodies break down the glucose from the food that we eat or drink, and this is released into the bloodstream.
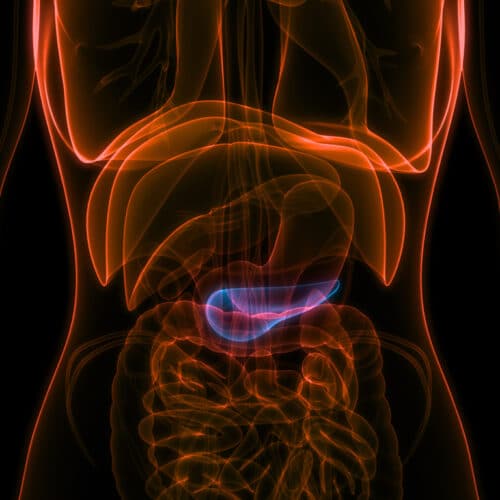
A hormone called insulin – which is produced by an organ called the pancreas – acts like a key to unlock the cells’ ability to absorb glucose from the bloodstream through the cell wall. The glucose that is absorbed is then used as energy. It is the pancreas that senses the right amount of the hormone insulin needed to be released for this whole process to function properly.
With diabetes, this process is faulty. There are two types of diabetes. Type 1 diabetes is a condition in which the pancreas produces little or no insulin, and it usually starts early in life. In Type 2 diabetes – which accounts for 95% of diabetes cases – cells stop recognising and responding to insulin, and this is referred to as insulin resistance.
With insulin resistance, glucose levels in the body rise after we have eaten, the pancreas detects the rising levels of glucose and produces more insulin to reduce glucose levels. When glucose levels continue building in the blood, this is referred to as glucose intolerance.
Is there a link between Parkinson’s and diabetes?
For a long time researchers have known that there is a close relationship between Parkinson’s and diabetes; a significant proportion of people with Parkinson’s have glucose intolerance and some also live with the added burden of diabetes.
Insulin also does its job of controlling glucose levels in the brain. Insulin has been shown to impact dopamine levels – dopamine is a chemical released in the brain and used to send messages between nerve cells. Research shows that insulin also helps with our cognitive function – the ability to think clearly, to learn, and remember. Notably, defects in insulin processes in the brain may contribute to Parkinson’s.
Research has suggested that people with diabetes are around 40% more likely to develop Parkinson’s than those without diabetes. In addition, individuals with Parkinson’s who are diabetic often have a more rapid progression of their symptoms, so careful management of both conditions is important.
Currently, one in 15 people in the UK has Type 2 diabetes, and that number is increasing; the risk of developing Parkinson’s in a person’s lifetime is also growing. Therefore, it is important that we try to understand the relationship between the two conditions, and whether certain Type 2 diabetes medications might, in turn, be able to slow the progression of Parkinson’s.
One common form of medication used in the treatment of diabetes is a class of drug called GLP-1R agonists.
GLP-1R agonists and Parkinson’s
Glucagon-like peptide 1 receptor agonists, or GLP-1R agonists, are a class of drugs that function by mimicking the action of naturally produced hormones in the gut called ‘incretins’. These gut hormones work by helping the body produce insulin when needed, they also reduce the amount of glucose released from where it is stored in the liver, they reduce the rate that the stomach digests food and empties, and can also reduce appetite. When eating food, the gut hormones stimulate the pancreas to release insulin needed to help cells absorb the glucose from our food. Receptors responding to these incretin gut hormones are present throughout the body including the brain. GLP-1R agonists act by increasing the action of the incretins or gut hormones in the body.
Many studies have shown that GLP-1R agonists actions in the brain occur in a variety of ways; effecting neurogenesis (the process by which new neurons are formed in the brain), improving energy function, and providing a supportive and protective effect. The first GLP-1R agonist approved for the treatment of diabetes was exenatide.
Previous assessments of the impact of GLP-1R agonists in Parkinson’s and funded by Cure Parkinson’s have indicated an association between people being treated with certain GLP-1R agonists for their diabetes, and a reduced risk of developing Parkinson’s
It’s important to note that the vast majority of people with diabetes do not develop Parkinson’s and similarly, the majority of people with Parkinson’s do not have a diagnosis of diabetes.
Q & A’s:
I have Parkinson’s – should I be taking GLP-1R agonists?
It is important to remember that GLP-1R agonists are currently considered an experimental class of drugs for Parkinson’s and much more research is needed before they are approved for use in Parkinson’s.
We advise that any adjustments to your current treatment regimes must be discussed with your clinician or neurologist.
Do all GLP-1R agonists used to treat Type 2 diabetes have the same effect in Parkinson’s?
There is a wide range of subtle differences between the broader class of GLP-1R agonists and they have not all been tested in Parkinson’s. Some GLP-1R agonists significantly reduce body weight (which might add concerns of frailty for people with Parkinson’s). Other GLP-1R agonists do not cross the blood brain barrier very well, and therefore are not able to have an effect in the brains of people with Parkinson’s. It is important to note that more research is required to better understand these differences in the context of a potential treatment for Parkinson’s.
How is Cure Parkinson’s actively advancing the progress of this potential therapy?
Cure Parkinson’s has focused its investment in supporting work on those GLP-1R agonists that can cross the blood brain barrier to have an effect – particularly lixisenatide, liraglutide and exenatide.
Cure Parkinson’s steered the first pilot study of exenatide in Parkinson’s and we are currently supporting the larger Phase 3 trial in people with Parkinson’s which will end in 2024. There is reason to believe exenatide could offer benefit in Parkinson’s as it may interrupt the biological pathways involved in the condition; the Phase 3 clinical trial of exenatide is evaluating whether it can slow the progression of Parkinson’s and will hopefully provide conclusive data.
Cure Parkinson’s has focused its funding to support work on those GLP-1R agonists that are brain penetrating, meaning these drugs can cross the blood brain barrier – particularly lixisenatide and exenatide. The first GLP-1R agonist tested in people with Parkinson’s was exenatide.
Evidence for the relationship between Type 2 diabetes and Parkinson’s
Diabetes and the risk of Parkinson's – read more Insuline resistance in undiagnosed people with Parkinson's – read more The Impact of Type 2 Diabetes in Parkinson's Disease Diabetic people taking diabetes medications and the risk of Parkinson's The neuroprotective effects of GLP-1 medications in Alzheimer's and Parkinson's
Phase 2 trial results of lixisenatide published
The full results of the one-year, phase 2 clinical trial of Type 2 diabetes drug lixisenatide have now been published. This Cure Parkinson’s co-funded trial has reported positive results,…

Spring Research Update meeting 2024: watch again
Our Spring Research Update Meeting once again took place at the renowned Royal Society of Medicine, Wimpole Street, London where we invited guests to an inspiring agenda of some…

Preliminary phase 2 trial results of lixisenatide presented
A one-year, phase 2 clinical trial of Type 2 diabetes drug lixisenatide has reported positive early results, which indicate that the treatment may slow the progression of motor (or…

The influence of diabetes on Parkinson’s progression
In recent research funded by Cure Parkinson’s, scientists have provided the strongest evidence to date that diabetes can affect the progression of Parkinson’s.

Liraglutide trial: results
Researchers from Cedars Sinai Hospital, Los Angeles have presented their initial top line results of the liraglutide trial, co-funded by Van Andel Institute and Cure Parkinson’s, at the recent…

Diabetes dual agonist drugs for Parkinson’s
Glucagon-like peptide 1 receptor (or GLP-1R) agonists are recognised as a frontline treatment for diabetes. Researchers have recently been developing the next generation of treatment for diabetes which target…

The exenatide phase 3 study protocol
Researchers conducting the phase 3 ‘Exenatide PD3’ clinical trial have published the protocol of the study, which outlines the details of the trial. Cure Parkinson’s is supporting two sub-studies…

Further support for diabetes treatments for Parkinson’s
A research group in South Korea has published results of their trial which provide further evidence that diabetes treatments can slow down the development of Parkinson’s in people with…
Further data on the relationship between diabetes and Parkinson’s
New research has found that there is convincing evidence that Type 2 diabetes is associated with a greater risk of Parkinson’s, but may in turn allow for better management…

Type 2 diabetes medications impact risk of Parkinson’s
In a recent study, researchers have concluded that the elevated risk of Parkinson’s in patients with type 2 diabetes might be mitigated depending on the type of drugs prescribed…

The liraglutide trial for people with Parkinson’s
This clinical trial will test the efficacy and safety of the diabetes drug liraglutide (a GLP-1 agonist) in people with Parkinson’s. The trial is taking place at the Cedars-Sinai…

Exenatide: further studies initiated
In 2012, Cure Parkinson’s initiated the International Linked Clinical Trials (iLCT) programme to focus on identifying and prioritising potentially disease-modifying therapies for Parkinson’s. The first drug to be prioritised…

New developments in diabetes drugs for Parkinson’s
At the forefront of treatments for diabetes is a class of drug called glucagon-like peptide 1 receptor (or GLP-1R) agonists. There is also now considerable laboratory research that suggests GLP-1R diabetes…

The Bydureon phase 3 trial: supplementary substudies
Cure Parkinson’s and Van Andel Institute (VAI) are delighted to be supporting two sub-studies within the important Bydureon phase 3 trial (Exenatide-PD 3)
