
Neuroinflammation
Inflammation is one of the body’s normal defense responses when it detects something unusual or dysfunctional. When the immune system identifies something it considers a ‘threat’ to its normal function, inflammation is a process by which the body can be alerted to the problem and the threat can be dealt with. However, when the body incorrectly identifies a problem or inflammation does not subside, it may lead to damage of normal cells. Neuroinflammation, or inflammation in the brain, is thought to be a factor in driving dopamine neuron (nerve cell) loss in Parkinson’s. Therefore, researchers are interested in whether medications which reduce inflammation (anti-inflammatory drugs) could slow Parkinson’s progression.
Anti-Inflammatory Molecules in Gut-First Parkinson’s
Dr Sandra Cardoso at the University of Coimbra, Portugal, is investigating if treating gut inflammation may prevent or slow Parkinson’s onset and progression. The idea that long-term gut inflammation may facilitate or initiate Parkinson’s development is referred to as “gut-first Parkinson’s”. It is understood that constipation is a common and early symptom of Parkinson’s. Additionally, there is a suggested association between inflammatory bowel diseases (IBD) and Parkinson’s.
Therefore, researchers are interested in whether gut issues are a facilitator of disease progression rather than a symptom. In this preclinical study, Dr Cardoso will examine this pathway by evaluating if anti-inflammatory molecules can reduce gut inflammation to subsequently reduce neuroinflammation and prevent Parkinson’s progression.
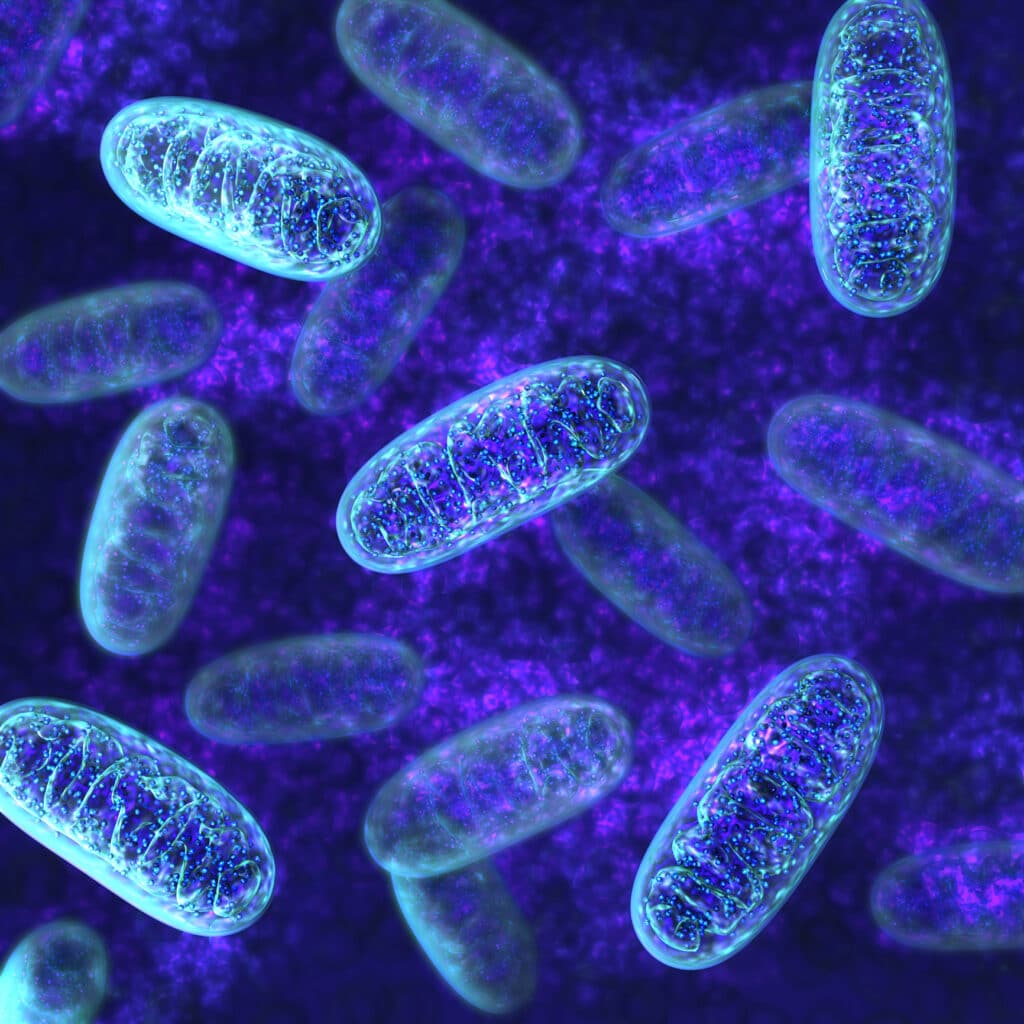
Mitochondrial Dysfunction
Another target for potentially disease-modifying therapies for Parkinson’s is the mitochondria. Mitochondria produce all the energy our cells need to function; however, in people with Parkinson’s, there are often problems with these tiny power stations. Without a stable energy supply, cells cannot survive meaning that mitochondrial dysfunction is considered a major driver of dopamine neuron loss in Parkinson’s. Therefore, if a drug can mitigate this dysfunction, it may be able to slow disease progression.
Anti-Gout
Professor Heather Mortiboys at the University of Sheffield is evaluating how two drugs, probenecid and thiosalicylic acid, used to treat gout (a form of inflammatory arthritis) may slow Parkinson’s progression by addressing mitochondrial dysfunction. These drugs appear to achieve this by promoting “mitophagy”, the process by which damaged or dysfunctional mitochondria are recycled in the cell. Mitophagy is a normal part of a cell’s lifecycle which may be reduced in people with Parkinson’s. The primary objective of this study is to gain a better understanding of how these drugs promote mitophagy, to evaluate if they promote the survival of dopamine neurons and to determine if they may be suitable for a future clinical trial.
Isradipine
Dr James Surmeier at Northwestern University is developing an intranasal formula (taken through the nose) for isradipine – a high blood pressure medication – for the treatment of Parkinson’s. Evidence suggests that isradipine may reduce mitochondrial stress in dopamine neurons, therefore mitigating neuron loss. Isradipine has been tested in two clinical trials for early-stage Parkinson’s; however, the results did not show any clinically significant outcomes. Further analyses of the results indicated that this may have been due to the amount of isradipine that was able to reach the brain when taken by mouth. Dr Surmeier’s team is investigating if the use of a nasal delivery could ensure a higher isradipine concentration reaching the brain and if this, in turn, can affect Parkinson’s progression.

Alpha-Synuclein
Dysfunctional copies of a protein known as alpha-synuclein are known to group together to form clumps (also known as Lewy bodies) in the dopamine producing neurons of people with Parkinson’s. If cells are unable to clear these clumps they become toxic to the cell and ultimately lead to cell death. The presence of this aggregated alphs-synuclein in dopamine neurons is a known hallmark of Parkinson’s and it is thought this may also contribute to their loss in people with the disease. Researchers are interested in finding therapies that reduce or prevent alpha-synuclein accumulation in order to slow or stop progression.
Rifabutin
Dr Lorraine Kalia at the University Health Network, Toronto is investigating whether an antibiotic, rifabutin, could be used as a disease-modifying treatment for Parkinson’s. Preclinical evidence suggests rifabutin may reduce alpha-synuclein accumulation by promoting waste clearance in the cell. Additionally, recent research has shown rifabutin has a significant, short-term effect in treating Crohn’s disease – an inflammatory bowel disease suggested to have an association with Parkinson’s. Dr Kalia’s lab will investigate what rifabutin interacts with in the cell to achieve its effect, as well as test a new method of measuring alpha-synuclein levels in cells to monitor Parkinson’s progression.





